Over the past few years, I have had the privilege to be surrounded by amazing, intelligent, and caring people. Nowhere was that more true than at Mass Academy, a small haven for those who took pleasure in exploring the inner workings of the world and the universe.
I’ve learned a few things from the experience of being surrounded by so many accomplished individuals. There are times when inklings of inadequacy spread like the flu. But with no symptoms, that feeling is invisible and internal. Nor is it unique—every single student feels the same, just in their own different way. The cure for this sickness is, in a way, quite simple. Yet the simple things can often be the most challenging to achieve in practice.
You need to be able to detach your own self-worth from that feeling of inadequacy, lest it become a dangerous, self-fulfilling prophecy. Solace doesn’t have to come from sheer willpower, but rather from community. Take part in it, for it transforms strangers into friends.
Today, elite institutions have come in to societal scrutiny for creating a modern version of dynastic inheritance. Certainly some of that scrutiny is deserved, as argued by Daniel Markovits in The Meritocracy Trap. The most subversive aspect of meritocracy as an institution, is that no one can argue that those very people did not work hard to get where they were. It’s just that they started with a number of advantages.
And so Mass Academy stands in a unique position. While its foundations share the same cement of meritocracy, it draws its water from a much purer source: its nature as a small and academically challenging public institution acts as a filter to bring only those with sincere dedication. The casting of such a wide net invites diversity of values scarcely found in other elite and therefore, wealthy institutions. One decisive consequence of this is that Mass Academy is, at heart, not competitive, but rather collaborative. The community it fosters is strangely harmonic, despite its disparate notes.
But that is slowly changing. In my conversation with a more recent student, also coming from St. John’s, he lamented at the insatiable desire for Mass Academy students to focus on grades and test scores, and very little else. This saddens me greatly, because Mass Academy is the perfect place to explore and grow. The school has an amazing opportunity, therefore, to open other avenues of character development through the arts.
I hope that Mass Academy doesn’t become a bubble, sucked into the measured accomplishments of the elite. It currently stands outside those measures, and I hope that it continues to produce students devoid of the darkness that such measures often imbue.
One critique I do have of Mass Academy is that well-roundedness, and character development, is often easily overlooked. With careful thought, Mass Academy can achieve the delicate balance of cultivating exceptional students in the scientific disciplines, as well as provide a breadth of experiences that develop the moral character of its students. It’s not there yet, but in my mind, that is its ultimate purpose.
I envision a day where the student that Mass Academy releases into the world is akin to the age-old ideal of the Renaissance Man. However, even that analogy is a bit limiting—the level of knowledge expected back then was far below what we now consider expertise. However, today, expertise isn’t all that necessary for a new generation of leaders. Rather being at the intersection of disciplines is what produces innovators in the modern world. Therefore I think that Mass Academy is perfectly position to produce such innovators.
I then expect it to bring in students from outside its traditional mathematics and science background; to cultivate a sense that breadth of understanding is today just as important as depth of understanding.
And while it can be argued either way whether or not Mass Academy counts as an “elite institution,” as defined by wealth and modern intellectual dynastic transmission, there is no doubt that colleges and universities are much easier to fit into the traditional descriptions.
Unfortunately, with each passing day, it becomes more and more impossible to escape the grasp of meritocratic hyper-competition. Even individualistic resolve to not become entrapped is met with resistance: “To be a parent is to be compromised. You pledge allegiance to justice for all, you swear that private attachments can rhyme with the public good, but when the choice comes down to your child or an abstraction—even the well-being of children you don’t know—you’ll betray your principles to the fierce unfairness of love.” As George Parker succinctly demonstrates, these mechanisms are self-reinforcing.
Elite ideals, as Elizabeth Currid-Halkett explains, “may seem completely innocent—perhaps even enlightened. Yet, as we discuss here, they simultaneously shore up inequality, erode social mobility, and create an ever-more stratified society—all without most of us noticing. This is a conversation that implicates us all, and, for that very reason, it is well worth addressing.”
And so the entirety of education begins to seem as simply an avenue into continued elite segregation, not by heritage or wealth, but by “merit.” Is that really any different?
From The Wall Street Journal’s article:
“The College Board plans to assign an adversity score to every student who takes the SAT to try to capture their social and economic background, jumping into the debate raging over race and class in college admissions.”
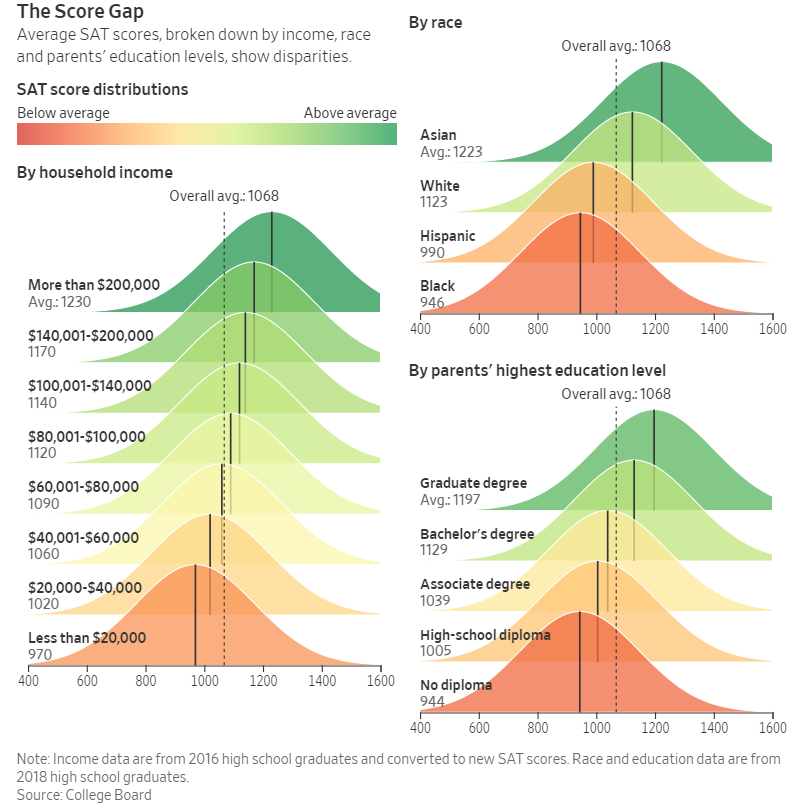
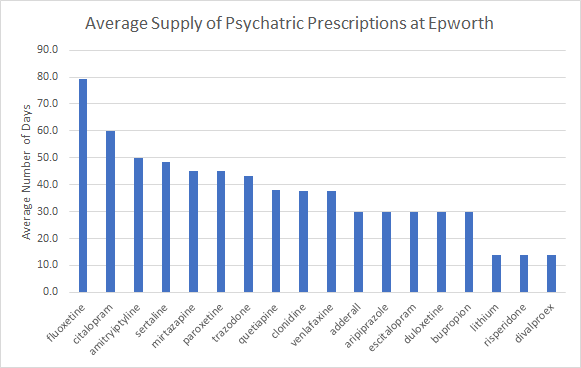
To be honest, I’m not entirely sure what difference the adversity score will make to college admissions. Certainly admissions processes have improved over the years (as argued by Markovits), but much remains to be done (as evidenced by the recent admissions scandals and lawsuits). At the same time, the score disparity has hardly been overcome, and in fact, only been amplified in recent years.
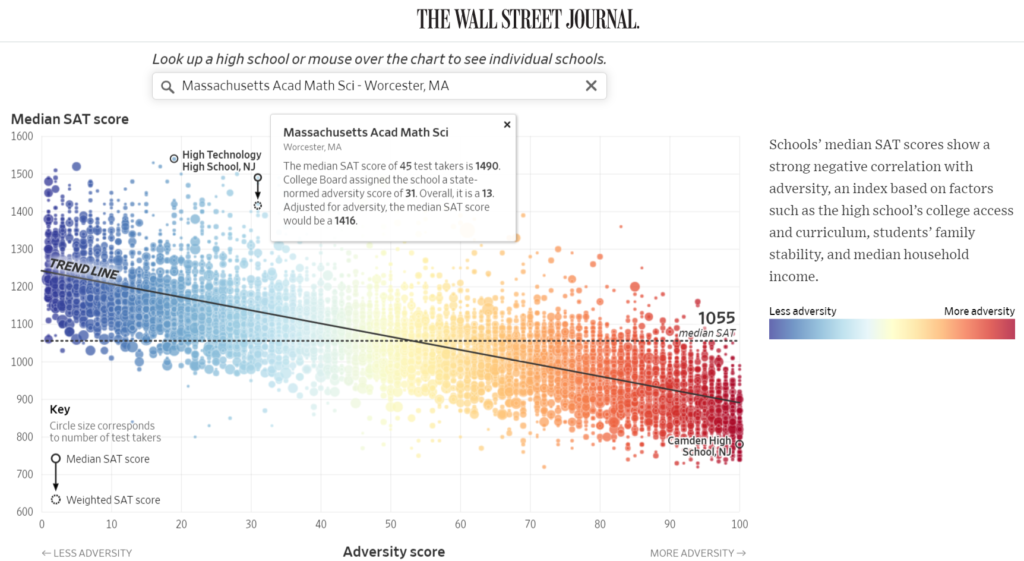
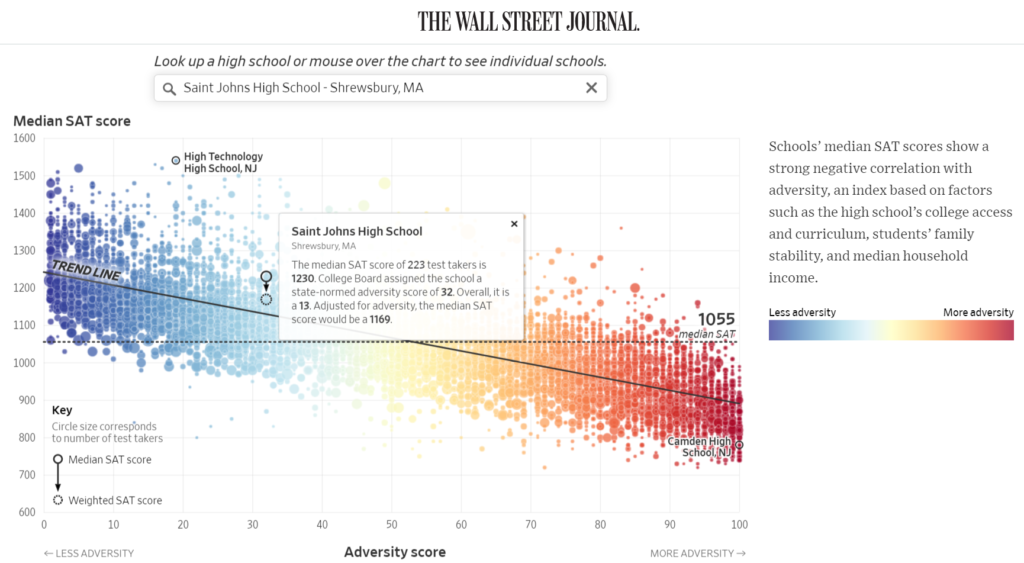
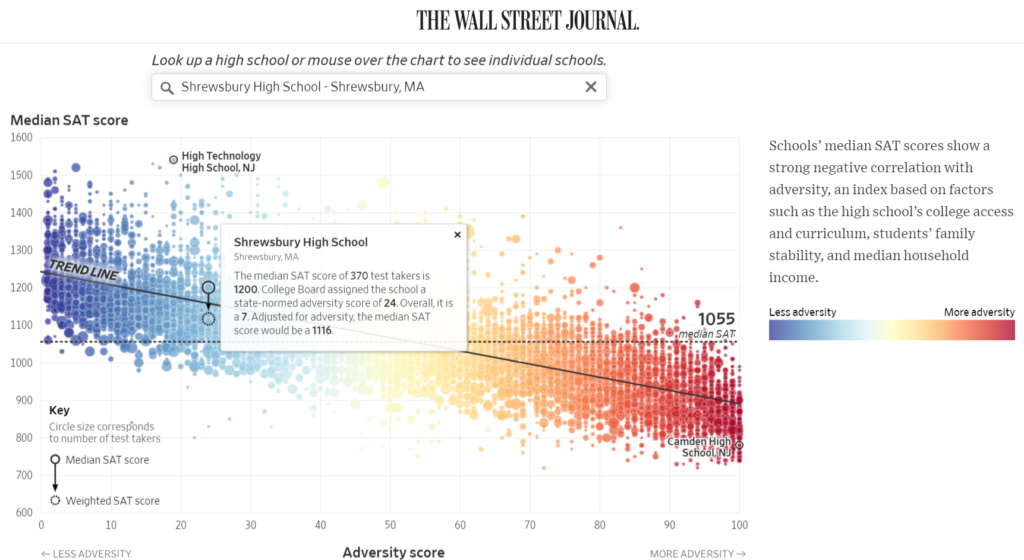
The differences in adversity scores for Mass Academy, Saint John’s, and Shrewsbury High, are non-trivial. But they don’t mean much in this context. Rather meaning is gleamed only by comparison across large gaps, where large-scale policy can make a difference.
Nonetheless, I am glad that I went to public school for my early education, then Catholic school for the first two years of high school, and then to Mass Academy for my final years of high school. It exposed me to an immense continuum of culture, and it made me deeply appreciate my background and upbringing in the intersection of so many cultures.
I know that this post was pulled in a few different directions, but ultimately, my point is simple: wherever you are, create a true community from the group of people you are surrounded by.
Dossier
“When the Culture War Comes for the Kids,” by George Packer, October 2019. https://www.theatlantic.com/magazine/archive/2019/10/when-the-culture-war-comes-for-the-kids/596668/
“SAT to Give Students ‘Adversity Score’ to Capture Social and Economic Background,” by Douglas Belkin, May 16, 2019. https://www.wsj.com/articles/sat-to-give-students-adversity-score-to-capture-social-and-economic-background-11557999000
“What Happens if SAT Scores Consider Adversity? Find Your School,” by Douglas Belkin, November 16, 2019. https://www.wsj.com/articles/what-happens-if-sat-scores-consider-adversity-11574773201
“The Meritocracy Trap,” by Daniel Markovits, September 10, 2019.
“How Whole Foods, yoga, and NPR became the hallmarks of the modern elite,” by Ezra Klein, November 14, 2019. https://www.vox.com/podcasts/2019/11/14/20964420/whole-foods-yoga-npr-elite-ezra-klein-elizabeth-currid-halkett-inequality
“The subtle ways colleges discriminate against poor students, explained with a cartoon,” by Alvin Chang, September 12, 2018. https://www.vox.com/2017/9/11/16270316/college-mobility-culture